Title: The Invisible Threat: How Smoking Elevates the Risk of Marginal Zone Lymphoma Transformation
Introduction
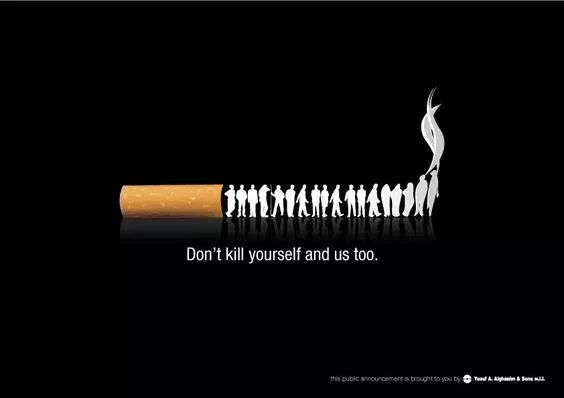
Marginal Zone Lymphoma (MZL) is a rare and indolent form of non-Hodgkin lymphoma, often characterized by a slow progression and relatively favorable prognosis. However, a significant concern in the management of MZL is the risk of transformation into a more aggressive lymphoma, such as diffuse large B-cell lymphoma (DLBCL), which drastically alters treatment strategies and diminishes survival outcomes. While genetic predispositions and chronic inflammatory conditions are well-recognized risk factors, emerging evidence underscores a modifiable behavioral risk: smoking. This article delves into the mechanistic pathways and epidemiological data linking smoking to an increased risk of MZL transformation, highlighting the urgent need for integrated smoking cessation strategies in lymphoma care.
Understanding Marginal Zone Lymphoma and Transformation
MZL arises from memory B-cells in the marginal zone of lymphoid tissues and is categorized into three subtypes: extranodal (MALT lymphoma), nodal, and splenic. Its indolent nature often allows for watchful waiting or localized therapies. Transformation, occurring in approximately 5-10% of cases, signifies a shift to a high-grade lymphoma, most commonly DLBCL. This event is associated with rapid symptom onset, resistance to conventional therapies, and a median survival of less than two years post-transformation. The triggers for transformation are multifaceted, involving genetic mutations (e.g., TP53, MYC), chronic antigen stimulation (e.g., H. pylori infection in gastric MALT), and immune dysregulation. Recent research has begun to pinpoint lifestyle factors, particularly smoking, as a critical accelerant in this malignant progression.
The Smoking-Lymphoma Nexus: Epidemiological Evidence
Several cohort and case-control studies have established a correlation between smoking and the incidence of various lymphomas, including MZL. A 2019 meta-analysis in the Journal of Clinical Oncology reported that current smokers had a 30% higher risk of developing MZL compared to never-smokers. More critically, longitudinal studies focusing on MZL patients have shown that active smoking at diagnosis is independently associated with a heightened risk of transformation.
For instance, a prospective study published in Blood Advances (2022) followed 620 MZL patients over a median of 8 years. It found that current smokers had a 2.5-fold increased risk of transformation to DLBCL compared to non-smokers, even after adjusting for age, subtype, and initial treatment. The risk exhibited a dose-response relationship, with heavy smokers (≥20 pack-years) facing the highest hazard ratio. Former smokers who had quit for more than a decade had a risk profile similar to never-smokers, suggesting that the detrimental effects might be reversible upon cessation.
Mechanistic Insights: How Smoking Fuels Lymphomagenesis and Progression
The carcinogenic properties of tobacco smoke, containing over 7,000 chemicals, including at least 70 known carcinogens like nitrosamines and polycyclic aromatic hydrocarbons (PAHs), directly contribute to lymphomagenesis and disease progression through several interconnected pathways:
Genomic Instability and Mutagenesis: Tobacco carcinogens are systemically absorbed and can directly damage DNA within B-cells. Benzopyrene, a key PAH, forms DNA adducts that lead to mutations in critical genes like TP53 and BCL6. These mutations are hallmark events in lymphomagenesis and are frequently observed in transformed DLBCL. The constant genotoxic stress from smoking provides a fertile ground for the acquisition of additional driver mutations that push indolent MZL clones toward aggression.
Chronic Immune Activation and Inflammation: Smoking induces a state of systemic inflammation. It elevates levels of pro-inflammatory cytokines such as TNF-α, IL-6, and IL-1β. This chronic inflammatory milieu provides continuous stimulation to B-cells, promoting their proliferation and survival. For MZL, which is often driven by chronic inflammatory or infectious triggers (e.g., H. pylori, hepatitis C), smoking acts as a potent co-factor, exacerbating the antigen-driven proliferation and increasing the statistical probability of a malignant clone acquiring transformative mutations.
Disruption of Immune Surveillance: A functional immune system is crucial for identifying and eliminating nascent cancerous cells. Smoking profoundly suppresses immune surveillance by impairing the function of natural killer (NK) cells and cytotoxic T-cells, which are vital for controlling B-cell malignancies. It also alters the tumor microenvironment, promoting the recruitment of immunosuppressive cells like myeloid-derived suppressor cells (MDSCs). This weakened defense mechanism allows transformed, aggressive lymphoma cells to proliferate unchecked.
Epigenetic Modifications: Beyond direct DNA damage, smoking induces epigenetic changes such as DNA methylation and histone modifications. Hypermethylation of tumor suppressor gene promoters can silence their expression, a common event in lymphoma progression. These epigenetic alterations can be heritable within cell clones, creating a permissive landscape for transformation that persists long after exposure.
Clinical Implications and the Role of Cessation
The link between smoking and MZL transformation has profound clinical implications. Oncology assessments must now rigorously include detailed smoking histories and pack-year calculations for all MZL patients. This risk factor should be incorporated into prognostic models to identify high-risk patients who might benefit from more vigilant monitoring or different therapeutic approaches.
Most importantly, these findings powerfully reinforce the necessity of smoking cessation as a integral component of cancer care. Oncologists, hematologists, and primary care physicians must provide structured cessation support—including counseling, nicotine replacement therapy (NRT), and pharmacotherapy (e.g., varenicline)—to patients diagnosed with MZL. The evidence that long-term quitters see their risk revert to baseline levels offers a powerful message of hope and agency to patients, empowering them to take a active role in improving their prognosis.
Conclusion
The transformation of Marginal Zone Lymphoma represents a catastrophic event in the disease course. While not all factors are within a patient's control, smoking stands out as a significant and modifiable risk factor. The robust epidemiological data, supported by a clear biological rationale, paint an undeniable picture: tobacco smoke acts as a potent accelerant in the progression from indolent to aggressive lymphoma. Integrating aggressive smoking cessation interventions into the standard management of MZL is not just a public health recommendation; it is a critical oncological strategy to mitigate risk, improve outcomes, and ultimately save lives. The goal is clear: to extinguish this invisible threat before it can fuel a more visible and dangerous disease.
Tags: #MarginalZoneLymphoma #LymphomaTransformation #SmokingAndCancer #Oncology #CancerResearch #SmokingCessation #DLBCL #CancerPrevention #LymphomaAwareness #TobaccoCarcinogenesis










