Title: Clearing the Air: How Smoking Fuels Chronic Sinusitis and Nasal Polyp Recurrence
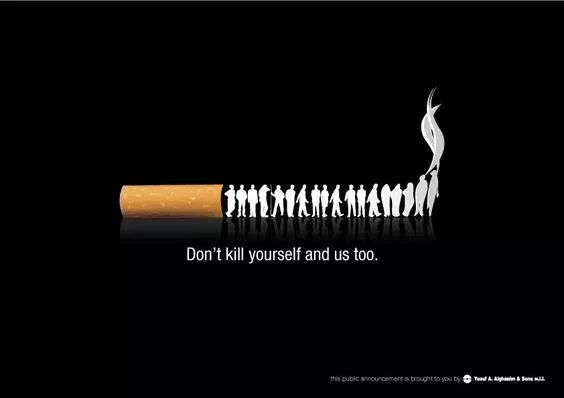
Chronic sinusitis with nasal polyps (CRSwNP) is a debilitating condition characterized by persistent inflammation of the sinuses and the growth of soft, non-cancerous swellings (polyps) in the nasal and sinus passages. For patients who undergo the immense relief of polyp removal surgery, the fear of recurrence is a constant shadow. While numerous factors influence this risk, a growing body of compelling evidence points to one major, modifiable culprit: smoking. The act of smoking, whether actively or through exposure to secondhand smoke, significantly elevates the recurrence rate of nasal polyps, creating a vicious cycle of inflammation, surgical intervention, and disappointment.
Understanding the Enemy: Chronic Sinusitis and Nasal Polyps
To appreciate smoking's role, one must first understand the pathology of CRSwNP. It is more than just a "stuffy nose"; it is a chronic inflammatory disorder. The linings of the sinuses become perpetually inflamed, leading to symptoms like facial pain and pressure, nasal congestion, reduced sense of smell (anosmia), and thick nasal discharge. Nasal polyps are a common complication of this inflammation. These grape-like structures obstruct the nasal airways and sinuses, exacerbating symptoms and often necessitating medical or surgical treatment.
The primary treatment goal is to reduce inflammation and restore airflow. This often involves long-term use of intranasal corticosteroids and, in many cases, functional endoscopic sinus surgery (FESS). FESS is highly effective at removing polyps and widening sinus openings, providing significant symptomatic relief. However, success is not always permanent. Recurrence rates are notoriously high, with studies showing polyp regrowth in a substantial percentage of patients within years of surgery.
The Inflammatory Onslaught: How Smoking Damages Sinus Health
Cigarette smoke is a toxic cocktail of over 7,000 chemicals, including nicotine, carbon monoxide, formaldehyde, and numerous other irritants and carcinogens. When inhaled, this smoke delivers a direct assault on the delicate mucosal lining of the upper airways, including the sinuses.
Direct Irritation and Epithelial Damage: The smoke physically and chemically irritates the ciliated epithelium—the layer of cells lining the sinuses that are responsible for trapping and moving mucus and pathogens out. This damage impairs the mucociliary clearance system, causing mucus to stagnate. This stagnant mucus becomes a breeding ground for bacteria and viruses, leading to repeated infections that fuel chronic inflammation.
Dysregulation of the Immune Response: Smoking profoundly disrupts the local immune environment in the sinonasal cavity. It:
- Promotes a Pro-Inflammatory State: Smoke exposure triggers the release of a flood of pro-inflammatory cytokines and signaling molecules, such as interleukin-1 (IL-1), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-α). This creates a state of constant, low-grade inflammation even in the absence of infection.
- Alters Immune Cell Function: It affects the behavior of key immune cells like neutrophils and eosinophils, often driving a type 2 inflammatory response, which is heavily implicated in nasal polyp formation.
- Impairs Barrier Function: The chemicals in smoke compromise the physical barrier of the sinus lining, making it more permeable to allergens and pathogens, which further stimulates the immune system.
This smoke-induced inflammation mirrors and amplifies the underlying inflammatory processes of CRSwNP, creating a perfect storm for disease persistence and severity.
The Link to Recurrence: From Inflammation to Regrowth
For a patient post-FESS, the surgical field is pristine but vulnerable. The goal is to maintain this state by controlling inflammation. Smoking directly sabotages this goal.
- Sustained Inflammatory Drive: The constant barrage of irritants from smoking ensures that the inflammatory environment that originally gave rise to the polyps remains active. This provides the ideal biochemical signals that encourage polyp tissue to regrow.
- Impaired Healing: Smoking vasoconstricts blood vessels, reducing blood flow and the delivery of oxygen and essential nutrients to the healing surgical site. This delays tissue repair and weakens the newly restored mucosal defenses, making it easier for inflammation to take hold again.
- Altered Microbiome: Research suggests smoking alters the microbiome of the nose and sinuses, potentially favoring colonies of bacteria that can perpetuate inflammation and contribute to polyp recurrence.
Clinical studies consistently back this mechanistic evidence. A meta-analysis published in the International Forum of Allergy & Rhinology concluded that both current and former smokers had a significantly higher risk of nasal polyp recurrence after endoscopic sinus surgery compared to never-smokers. The risk was dose-dependent, meaning heavier smokers faced an even greater likelihood of needing revision surgery.
Secondhand Smoke: The Invisible Threat
The danger is not confined to active smokers. Chronic exposure to secondhand smoke, particularly in children or adults living with a smoker, has also been linked to an increased incidence of chronic rhinosinusitis and worse postoperative outcomes. The involuntary inhalation of sidestream smoke exposes the sinuses to the same harmful cocktail of irritants, triggering inflammation and increasing the risk of polyp development and recurrence.
A Path Forward: Cessation as a Critical Treatment Pillar
The undeniable link between smoking and nasal polyp recurrence transforms smoking cessation from a general health recommendation into a specific, non-negotiable component of CRSwNP management. For patients considering or recovering from sinus surgery, quitting smoking is arguably as important as the surgery itself for long-term success.
Otolaryngologists now emphasize smoking cessation counseling as a standard of care. The benefits are profound:
- Reduced Inflammation: Cessation allows the inflammatory environment to calm down significantly.
- Restored Mucociliary Clearance: The cilia begin to recover function, improving mucus clearance and reducing infection risk.
- Improved Surgical Outcomes: Patients who quit smoking before surgery experience better healing, fewer complications, and a dramatically lower chance of polyp recurrence.
Support through counseling, nicotine replacement therapy, and other medical aids can greatly increase the chances of successful quitting.
Conclusion
The journey with chronic sinusitis and nasal polyps is challenging enough without adding a preventable risk factor. Smoking acts as a powerful accelerant, pouring fuel on the fires of inflammation that drive this disease and its frustrating tendency to return after treatment. Acknowledging the robust scientific evidence is the first step. For patients and clinicians alike, prioritizing smoking cessation is not merely an add-on but a fundamental strategy to break the cycle of recurrence, preserve surgical gains, and finally achieve lasting relief and improved quality of life.
Tags: #ChronicSinusitis #NasalPolyps #SmokingCessation #SinusHealth #ENT #Rhinology #SinusSurgery #Inflammation #PublicHealth #Tobacco










