Title: The Impact of Smoking on Functional Residual Capacity Percentage: Mechanisms and Health Implications
Introduction
Smoking remains one of the most significant public health challenges globally, contributing to a wide range of respiratory, cardiovascular, and systemic diseases. Among its many detrimental effects on the respiratory system, smoking has been shown to alter lung volumes and capacities, including the functional residual capacity (FRC). FRC refers to the volume of air remaining in the lungs after a normal, passive exhalation. It is a critical parameter in respiratory physiology, as it helps maintain alveolar stability, facilitates gas exchange, and influences lung compliance. This article explores how smoking raises the percentage of FRC, the underlying mechanisms, and the broader health implications of this change.
Understanding Functional Residual Capacity (FRC)
Functional residual capacity is the sum of expiratory reserve volume (ERV) and residual volume (RV). It represents the equilibrium point where the inward elastic recoil of the lungs is balanced by the outward chest wall recoil. FRC is typically measured using techniques such as body plethysmography, helium dilution, or nitrogen washout. In healthy individuals, FRC accounts for approximately 40% of total lung capacity (TLC) and plays a vital role in optimizing oxygen and carbon dioxide exchange during the breathing cycle. Alterations in FRC can indicate underlying respiratory pathologies, such as obstructive or restrictive lung diseases.
How Smoking Affects Lung Mechanics
Smoking introduces a complex mixture of over 7,000 chemicals, including nicotine, tar, carbon monoxide, and oxidative agents, into the respiratory system. These substances provoke chronic inflammation, oxidative stress, and structural changes in the airways and lung parenchyma. One of the primary effects of smoking is the destruction of elastic fibers in the alveoli, leading to emphysema—a hallmark of chronic obstructive pulmonary disease (COPD). Emphysema reduces lung elastic recoil, causing air trapping and hyperinflation. Consequently, the lungs lose their ability to deflate fully during exhalation, resulting in an increased residual volume (RV) and, by extension, an elevated FRC.
Additionally, smoking induces chronic bronchitis, characterized by inflammation and mucus hypersecretion in the bronchial tubes. This narrows the airways and increases resistance during expiration, further contributing to air trapping. The combined effects of emphysema and chronic bronchitis alter the pressure-volume relationship of the lungs, shifting the equilibrium point of FRC to a higher volume.
Evidence Linking Smoking to Elevated FRC Percentage
Numerous studies have demonstrated that smokers, even those without overt COPD, exhibit higher FRC percentages compared to non-smokers. For instance, a longitudinal study published in the American Journal of Respiratory and Critical Care Medicine found that current smokers had a 5–10% higher FRC than never-smokers, after adjusting for age, height, and gender. This increase was correlated with pack-years of smoking, suggesting a dose-response relationship. Another study using computed tomography (CT) imaging revealed that smokers with preserved spirometry often show signs of regional hyperinflation, consistent with elevated FRC.
The rise in FRC percentage is particularly pronounced in individuals with early-stage COPD, where hyperinflation compensates for airflow limitation to maintain ventilation. However, even in asymptomatic smokers, subclinical changes in lung mechanics can be detected through advanced pulmonary function tests.
Pathophysiological Mechanisms
The mechanisms through smoking raises FRC percentage are multifactorial:
-
Loss of Elastic Recoil: Proteolytic enzymes (e.g., elastase) released by neutrophils and macrophages in response to smoke-induced inflammation degrade elastin in alveolar walls. This reduces the lungs' ability to recoil, leading to passive expansion and increased FRC.
-
Airway Obstruction: Chronic inflammation and mucus plugging narrow the small airways, increasing resistance during expiration. This causes air to be trapped distally, elevating RV and FRC.
-
Altered Surfactant Function: Smoking disrupts the production and function of pulmonary surfactant, which reduces surface tension and prevents alveolar collapse. Dysfunctional surfactant promotes atelectasis and compensatory hyperinflation.
-
Neuroregulatory Changes: Nicotine and other chemicals affect the autonomic nervous system, potentially altering bronchomotor tone and breathing patterns, which may contribute to air trapping.
Clinical and Functional Implications
An elevated FRC percentage is not merely a numerical deviation; it has profound clinical consequences. Hyperinflation increases the work of breathing, as respiratory muscles operate at less efficient lengths. This leads to dyspnea (shortness of breath), especially during physical exertion, reducing exercise tolerance and quality of life. Over time, compensatory mechanisms fail, and hyperinflation progresses, exacerbating ventilatory limitations and increasing the risk of respiratory failure.
Moreover, hyperinflation impairs cardiac function by reducing venous return and increasing pulmonary vascular resistance, which can lead to cor pulmonale (right heart failure) in advanced cases. The increased FRC also compromises gas exchange; although lung volumes are larger, ventilation-perfusion mismatch worsens, contributing to hypoxemia and hypercapnia.
Public Health Perspective and Prevention
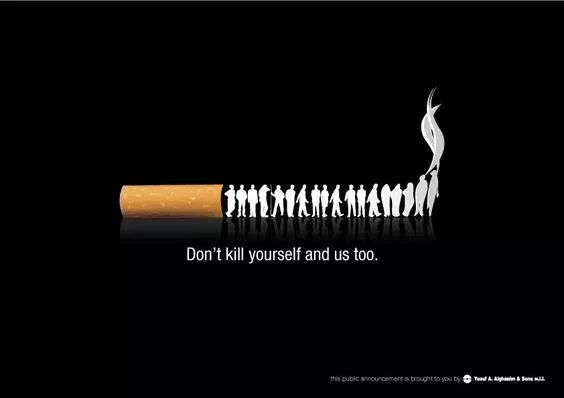
Given that smoking is the leading preventable cause of elevated FRC and associated diseases, public health interventions are crucial. Smoking cessation programs, regulatory measures (e.g., smoke-free laws), and public awareness campaigns can reduce smoking prevalence. Early detection through spirometry and lung volume assessments in high-risk individuals may help identify pathological changes before symptomatic disease develops.
Conclusion
Smoking significantly raises the functional residual capacity percentage through mechanisms involving loss of elastic recoil, airway obstruction, surfactant dysfunction, and neuroregulatory changes. This alteration in lung mechanics is an early indicator of smoke-induced lung damage and heralds the development of debilitating conditions like COPD. Understanding and addressing this issue through prevention, early intervention, and smoking cessation is essential to mitigate the global burden of smoking-related respiratory diseases.
Tags: Smoking, Functional Residual Capacity, Lung Volumes, Respiratory Physiology, COPD, Hyperinflation, Pulmonary Function, Public Health














