The Unseen Link: How Tobacco Use Can Prolong Antibiotic Treatment in Kidney Infections
When you're diagnosed with a kidney infection, medically known as pyelonephritis, the immediate goal is clear: start a potent course of antibiotics and eradicate the invading bacteria as quickly as possible. Both patients and doctors share this singular focus. However, a critical and often overlooked factor can silently undermine this entire effort—tobacco use. Emerging clinical insights suggest a troubling connection: smoking and tobacco consumption can significantly prolong the necessary duration of antibiotic therapy for pyelonephritis, turning a standard treatment into a protracted battle.
To understand this, we must first grasp what pyelonephritis entails. It's not a simple bladder infection; it's a serious condition where a urinary tract infection (UTI) has traveled upstream to one or both kidneys. The symptoms are severe—high fever, chills, intense back or flank pain, nausea, and a general feeling of being profoundly unwell. This isn't an ailment to be taken lightly; it requires prompt and effective medical intervention, typically with a tailored course of powerful antibiotics. The standard antibiotic treatment for pyelonephritis is designed to be robust, but its success hinges on the body's ability to work in concert with the medication.
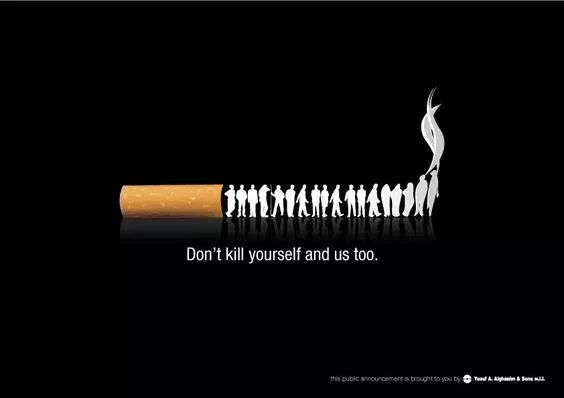
This is where tobacco enters the picture, not as a mere bad habit, but as a active physiological disruptor. The chemicals in tobacco smoke—nicotine, carbon monoxide, and thousands of other toxins—wage a silent war on the body's defense and repair systems on multiple fronts.
The Vascular Assault: Starving the Battlefield
One of the most direct ways tobacco use affects UTI treatment is through its devastating impact on the circulatory system. Nicotine is a potent vasoconstrictor, meaning it causes blood vessels to narrow. To fight a deep-seated infection like pyelonephritis, the body needs to deliver a high concentration of antibiotics and infection-fighting white blood cells directly to the kidneys. This requires robust blood flow. When tobacco-induced vasoconstriction occurs, it's like reducing the number of highways leading to the battlefield. The antibiotics and immune cells face a traffic jam, struggling to reach the infected tissues in sufficient numbers. This impaired drug delivery to infected kidneys means that even though you're taking your medication correctly, it might not be reaching its target at the optimal concentration, reducing its efficacy from the very start.
Furthermore, the kidneys themselves are highly vascular organs, reliant on a rich network of capillaries to function and heal. Tobacco smoke damages this delicate vasculature, compromising the organ's inherent ability to recover from the inflammatory damage caused by the infection. This impact of smoking on kidney infection recovery creates a double jeopardy: the medicine has a harder time arriving, and the organ itself is less capable of healing.
Weakening the Immune Army
Beyond the vascular system, tobacco smoke systematically dismantles key components of the immune system. Our lungs are not just for breathing; they house immune sentinels called alveolar macrophages, which are crucial for engulfing and destroying pathogens. Tobacco smoke paralyzes these cells. When bacteria from a kidney infection occasionally seed into the bloodstream (a condition called bacteremia), a weakened lung-based defense system is less able to clear them, potentially leading to complications.
Moreover, smoking reduces the levels of vital immunoglobulins—the antibodies that specifically target bacteria. It also impairs the function of neutrophils, the front-line infantry of the immune system. In a patient with pyelonephritis, whose body is already marshaling all its resources to fight a severe infection, tobacco use is akin to sending troops into battle malnourished and with faulty equipment. This state of smoking-induced immunocompromised state directly contributes to a prolonged UTI antibiotic course, as the body simply cannot mount an effective auxiliary attack to support the work of the antibiotics.
The Altered Microbiome and Biofilm Haven
The human body is a complex ecosystem, and the balance of bacteria, even the beneficial ones, is crucial for health. Smoking alters this microbiome, not just in the lungs but throughout the body, potentially creating an environment more hospitable to pathogenic bacteria. More insidiously, there is evidence that the inflammatory environment fostered by tobacco use can encourage bacteria to form biofilms.
Think of a biofilm as a fortress that bacteria build around themselves. It's a slimy, protective layer that makes it incredibly difficult for antibiotics to penetrate and kill the bacteria inside. If the bacteria causing pyelonephritis form a biofilm in the kidney, the infection becomes exponentially harder to treat. This can lead to recurrent pyelonephritis and smoking, creating a vicious cycle where each infection is more persistent than the last. This scenario of managing complex UTI with tobacco use often forces physicians to extend antibiotic treatment for pyelonephritis far beyond the standard protocol, sometimes switching to stronger, more invasive intravenous antibiotics for a longer duration.
Clinical Consequences: From Days to Weeks
So, what does this mean in practical terms for a patient? A typical case of uncomplicated pyelonephritis in a healthy non-smoker might require a 7 to 14-day course of oral antibiotics. For a smoker, the same initial diagnosis could easily evolve into a more complicated scenario.
Doctors may find that after the standard course, symptoms haven't fully resolved. Blood tests might show persistent inflammation, or a repeat urine culture may still show bacterial growth. This is the direct result of the mechanisms described above. Consequently, the physician has no choice but to extend the antibiotic regimen. This prolonged UTI antibiotic course increases the total antibiotic use duration for pyelonephritis, carrying its own set of risks.
Longer antibiotic exposure raises the likelihood of side effects like gastrointestinal distress (e.g., C. difficile infection), yeast infections, and drug-specific reactions. It also contributes to the global crisis of antibiotic resistance. When bacteria are exposed to sub-optimal levels of antibiotics for longer periods—a situation more likely with impaired drug delivery—it gives them a chance to develop resistance mechanisms, making future infections even harder to treat.
Furthermore, the impact of smoking on kidney infection recovery isn't just about the infection itself. Smoking is a primary risk factor for chronic kidney disease (CKD). A bout of pyelonephritis causes acute inflammation and scarring in the kidney. In a smoker, whose kidneys are already under constant assault from tobacco toxins, this acute insult can cause more significant long-term damage, accelerating the decline towards compromised kidney function.
A Path to Better Outcomes
The silver lining in this challenging situation is that it offers a powerful, actionable intervention point. Quitting tobacco is one of the most significant steps a patient can take to actively participate in their own healing. The benefits of cessation begin almost immediately. Within weeks, circulation improves, allowing for better antibiotic delivery. Within months, immune function begins to recover significantly.
For a patient diagnosed with pyelonephritis, addressing tobacco use isn't a sidebar conversation about long-term health; it is an integral part of the acute treatment strategy. Doctors should frame it as such: "To give these antibiotics the best chance to work quickly and effectively, and to prevent this from happening again, we need to talk about supporting you to quit smoking." This approach integrates managing complex UTI with tobacco use by tackling the root cause of the complication.
In conclusion, the connection between tobacco and a prolonged battle with pyelonephritis is a stark reminder that our lifestyle choices are deeply intertwined with our medical outcomes. Tobacco use doesn't just cause cancer or heart disease decades down the line; it actively interferes with the body's ability to fight acute, serious infections today. By recognizing that tobacco use affects UTI treatment by impairing drug delivery, suppressing immunity, and promoting harder-to-treat infections, we can better support patients through their recovery. For anyone facing a kidney infection, quitting tobacco is not just a healthy choice—it is a critical part of the prescription for a swift and complete recovery.