Tobacco Exposure Significantly Worsens Hemolytic Uremic Syndrome Prognosis
Abstract
Hemolytic Uremic Syndrome (HUS) is a severe thrombotic microangiopathy characterized by the triad of microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury. While the primary triggers, such as Shiga toxin-producing E. coli (STEC) infections, are well-established, the role of modifiable patient factors, particularly tobacco exposure, in influencing disease severity and long-term outcomes is increasingly recognized. This article examines the pathophysiological mechanisms through which tobacco smoke and nicotine exacerbate the vascular endothelial damage central to HUS, leading to more severe clinical presentations, higher complication rates, and poorer renal and overall survival. The evidence underscores the critical importance of smoking cessation as an integral component of HUS management and prevention strategies.
Introduction
Hemolytic Uremic Syndrome represents a medical emergency, most commonly affecting children following STEC infections, though atypical forms (aHUS) linked to complement dysregulation also occur. The prognosis of HUS has improved with advanced supportive care, including dialysis and plasma exchange, yet a significant proportion of patients suffer from chronic kidney disease (CKD), hypertension, and end-stage renal disease (ESRD) years after the acute episode. Identifying factors that aggravate the prognosis is paramount for improving patient outcomes. Among these, tobacco exposure stands out as a potent, yet preventable, aggravating factor that directly targets the vascular system, amplifying the very damage that defines HUS.
Pathophysiology of HUS: A Primer on Endothelial Insult
At its core, HUS is a disease of the endothelium. In typical HUS, Shiga toxin binds to globotriaosylceramide (Gb3) receptors on the surface of endothelial cells, particularly in the glomeruli. This binding triggers a cascade of events: inhibition of protein synthesis, upregulation of pro-inflammatory cytokines, and induction of apoptosis. The result is a pro-thrombotic state where platelets adhere to the damaged vessel walls, forming microthrombi that shearing passing red blood cells (hemolysis), consume platelets (thrombocytopenia), and obstruct blood flow, leading to ischemic organ damage, most notably in the kidneys.
In atypical HUS, uncontrolled activation of the complement alternative pathway causes identical endothelial injury and thrombotic microangiopathy. It is upon this foundation of profound endothelial dysfunction that tobacco smoke exerts its deleterious effects.
How Tobacco Smoke Exacerbates HUS Pathogenesis
Tobacco smoke contains over 7,000 chemicals, including nicotine, carbon monoxide, and oxidative stressors, which synergistically worsen the vascular injury in HUS through several interconnected mechanisms:
1. Amplification of Endothelial Dysfunction and Activation
Nicotine and other constituents directly damage the endothelium, reducing the production of protective vasodilators like nitric oxide (NO) and increasing the secretion of endothelin-1, a potent vasoconstrictor. This creates a state of vasoconstriction and heightened endothelial activation. In a patient with HUS, whose endothelium is already under severe attack, tobacco exposure adds a significant second hit, pushing the system toward more widespread and severe thrombotic complications.
2. Enhancement of Pro-thrombotic Milieu
Tobacco smoke increases platelet aggregation and adhesiveness, making platelets more likely to form clots. It also elevates levels of fibrinogen and other clotting factors. This pro-thrombotic shift directly fuels the formation of the microscopic clots that characterize HUS, potentially increasing their burden and distribution.
3. Induction of Oxidative Stress and Inflammation
The abundant free radicals in tobacco smoke cause significant oxidative stress, which further injures endothelial cells and promotes inflammation. This oxidative stress amplifies the inflammatory response already initiated by Shiga toxin or complement activation, leading to a more pronounced cytokine storm. This heightened inflammatory state can worsen organ damage, not only in the kidneys but also in the brain (increasing the risk of neurological complications like seizures or stroke) and the cardiovascular system.
4. Aggravation of Renal Vasoconstriction and Ischemia
Nicotine-induced vasoconstriction is particularly detrimental to the kidneys. It reduces renal blood flow and glomerular filtration rate (GFR), exacerbating the acute kidney injury at the heart of HUS. The resulting intensified ischemia can lead to more extensive cortical necrosis, a severe form of damage that dramatically reduces the chance of renal recovery.
Clinical Implications: From Presentation to Long-Term Prognosis
The biological mechanisms translate into stark clinical realities for HUS patients with a history of tobacco exposure, whether active or passive.
- More Severe Acute Presentation: Studies and clinical observations suggest these patients often present with lower platelet counts, higher serum creatinine levels (indicating worse kidney function), and a greater need for dialysis from the outset.
- Higher Rate of Complications: The risk of extra-renal complications, such as severe colitis, pancreatitis, and central nervous system involvement, is elevated. The compounded cardiovascular stress can also lead to hypertension and heart failure more frequently.
- Poorer Renal Recovery: The single most significant impact is on long-term renal survival. The additive endothelial and ischemic injury from tobacco smoke makes complete recovery of kidney function less likely. Patients are at a significantly higher risk of progressing to chronic kidney disease (CKD), requiring long-term dialysis or kidney transplantation.
- Increased Mortality: The overall burden of disease contributes to a higher mortality rate during the acute phase and in the years following due to renal and cardiovascular sequelae.
The Critical Role of Smoking Cessation
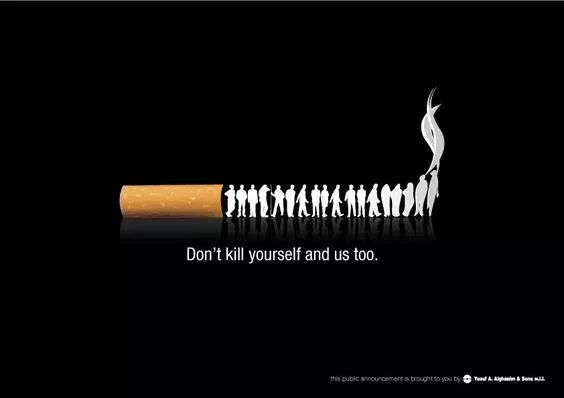
This dire prognosis highlights a crucial opportunity for intervention. Smoking cessation must be framed not as a general lifestyle recommendation, but as a specific, non-pharmacological therapeutic strategy for patients with or recovering from HUS. For patients with a history of HUS, avoiding tobacco in any form is essential to preserving residual renal function. For the broader population, especially parents of young children (the most common HUS demographic), understanding that exposure to secondhand smoke can similarly worsen outcomes provides a powerful incentive to maintain a smoke-free environment.
Conclusion
The evidence is clear: tobacco exposure is a major modifiable risk factor that significantly worsens the prognosis of Hemolytic Uremic Syndrome. It acts by exacerbating the underlying endothelial damage, promoting thrombosis, and intensifying renal ischemia, leading to more severe acute illness and devastating long-term consequences. Integrating aggressive smoking cessation counseling and support into the multidisciplinary management of HUS patients is no longer optional; it is an essential component of care aimed at salvaging kidney function and saving lives. Healthcare providers must unequivocally communicate this risk and empower patients and their families to make changes that can dramatically alter the disease trajectory.














