Smoking Exacerbates Sleep Apnea Severity: An Unseen Respiratory Burden
Abstract
The relationship between tobacco smoking and respiratory disease is well-established, yet its specific impact on the severity of sleep-disordered breathing remains a critical area of investigation. This article examines the compelling evidence linking cigarette smoking to an increased severity of the Apnea-Hypopnea Index (AHI), the primary metric for diagnosing and grading obstructive sleep apnea (OSA). By exploring the pathophysiological mechanisms—including upper airway inflammation, neuromuscular dysfunction, and sleep architecture disruption—we elucidate how smoking acts as a potent aggravating factor. Furthermore, this piece discusses the clinical implications of these findings, emphasizing that smoking cessation must be a cornerstone of OSA management protocols to improve patient outcomes and reduce the overall disease burden.
Introduction: Understanding AHI and OSA
Obstructive Sleep Apnea (OSA) is a prevalent disorder characterized by recurrent collapse of the upper airway during sleep, leading to apneas (complete cessation of airflow) and hypopneas (partial reduction in airflow). The Apnea-Hypopnea Index (AHI) is the gold standard for quantifying OSA severity, representing the average number of apneic and hypopneic events per hour of sleep. An AHI of 5-15 is classified as mild, 15-30 as moderate, and greater than 30 as severe OSA. While obesity, male gender, and age are recognized risk factors, emerging research underscores cigarette smoking as a significant and modifiable contributor that directly worsens AHI scores.
The Pathophysiological Nexus: How Smoking Worsens AHI
The detrimental effects of smoking on the respiratory system extend far beyond the lungs, directly targeting the structures and functions that maintain airway patency during sleep.
1. Upper Airway Inflammation and Edema
Cigarette smoke is a potent irritant containing thousands of toxic chemicals. Chronic inhalation leads to persistent inflammation and edema in the mucosal lining of the upper airway, including the soft palate, uvula, and pharynx. This swelling physically narrows the airway lumen, making it more susceptible to collapse under the negative pressure generated during inspiration in sleep. This structural narrowing directly increases the frequency of obstructive events, thereby elevating the AHI.
2. Impaired Neuromuscular Function
The patency of the upper airway is actively maintained by a complex interplay of muscles, including the genioglossus. These muscles receive neural signals to stiffen and contract during inspiration to counter collapse. Research indicates that nicotine and other smoke constituents can disrupt this protective reflex. They may alter the function of sensory receptors in the pharynx, blunting the neuromuscular response to airway obstruction. This impairment diminishes the body's ability to prevent apneas, leading to a higher AHI.
3. Sleep Architecture Disruption and Arousal Threshold
Nicotine is a powerful stimulant. Smokers often experience disrupted sleep architecture, including prolonged sleep latency, reduced total sleep time, and decreased slow-wave and REM sleep. While this might seem contradictory, fragmented sleep can paradoxically worsen OSA. Lighter sleep stages are more vulnerable to airway collapse. Furthermore, smoking may lower the arousal threshold, meaning the brain wakes up too easily in response to minor respiratory events that would not normally cause arousal. While this prevents longer apneas, it fragments sleep and contributes to the counting of more hypopneic events per hour, increasing the AHI.
4. Concomitant Lung Disease and Nocturnal Hypoxia
Smokers frequently develop chronic obstructive pulmonary disease (COPD) and chronic bronchitis. The overlap of OSA and COPD, termed "overlap syndrome," is particularly severe. Smoking-induced lung damage reduces overall lung volume, which in turn diminishes the tracheal tug on the upper airway, a stabilizing force. This loss of traction makes the airway more collapsible. Additionally, pre-existing damage from smoking lowers baseline oxygen saturation, meaning that each apnea or hypopnea results in more profound nocturnal hypoxia, amplifying the cardiovascular stress associated with a high AHI.
Epidemiological and Clinical Evidence
Numerous cross-sectional and cohort studies have consistently demonstrated a positive correlation between smoking status and AHI severity. Current smokers have been shown to have a significantly higher AHI compared to never-smokers, even after adjusting for confounders like age, gender, and body mass index (BMI). Importantly, former smokers often exhibit an intermediate risk, suggesting that while damage may be partially reversible, the effects can persist. Clinical polysomnography (sleep study) data repeatedly confirms that smokers present with more severe oxygen desaturation patterns and a higher respiratory disturbance index, a close correlate of AHI.
Conclusion and Clinical Implications
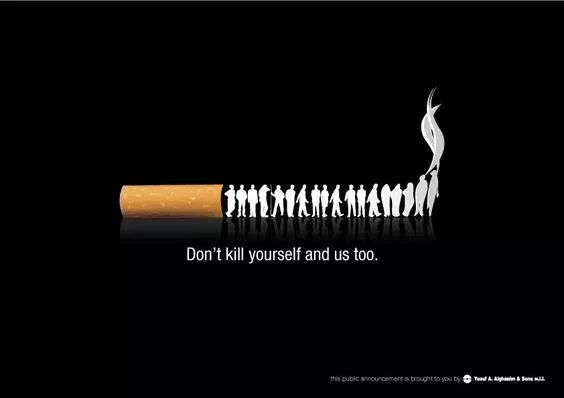
The evidence is conclusive: smoking is a major exacerbating factor for OSA severity, directly contributing to a higher Apnea-Hypopnea Index through multiple interconnected biological pathways. This relationship mandates a paradigm shift in clinical practice. For patients diagnosed with or at risk for OSA, screening for smoking history must be routine. Conversely, patients who smoke should be counseled on their elevated risk for sleep-disordered breathing.
Most critically, smoking cessation counseling should be integrated into every OSA treatment plan, alongside standard therapies like Continuous Positive Airway Pressure (CPAP). Quitting smoking can reduce upper airway inflammation, improve neuromuscular function, and stabilize sleep architecture, ultimately leading to a tangible reduction in AHI. Addressing this modifiable risk factor is not merely an adjunct therapy but a fundamental component of comprehensive care, offering a powerful opportunity to alleviate disease severity and enhance long-term health for millions affected by sleep apnea.











