Title: Tobacco Use Elevates the Risk of Ventricular Tachycardia in Pulmonary Heart Disease
Introduction
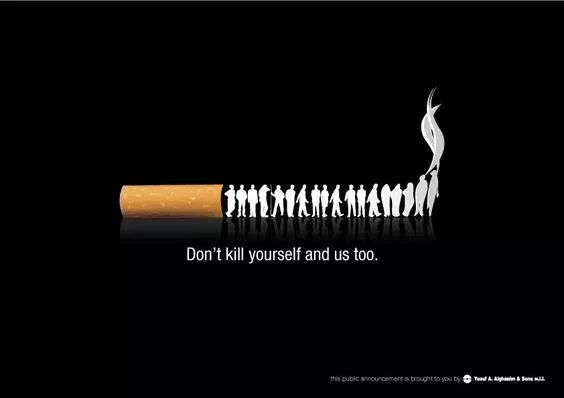
Tobacco use remains one of the leading preventable causes of death and disability worldwide. While its association with lung cancer and chronic obstructive pulmonary disease (COPD) is widely recognized, its profound impact on cardiovascular health, particularly in the development and exacerbation of pulmonary heart disease (PHD) and associated arrhythmias like ventricular tachycardia (VT), is equally critical yet often underemphasized. Pulmonary heart disease, also known as cor pulmonale, is a condition characterized by right ventricular enlargement and eventual failure due to disorders that affect the lungs, pulmonary vasculature, or breathing mechanics. A particularly lethal complication of this condition is the onset of ventricular tachycardia, a rapid, life-threatening heart rhythm originating from the ventricles. This article delves into the mechanistic pathways through which tobacco smoke significantly raises the incidence of ventricular tachycardia in individuals with pulmonary heart disease, exploring the interplay of hypoxia, inflammation, autonomic dysfunction, and direct cardiotoxicity.
The Pathophysiological Nexus: Tobacco, PHD, and VT
The pathway from tobacco consumption to ventricular tachycardia in the context of pulmonary heart disease is multifactorial, involving a vicious cycle of pulmonary and cardiac damage.
1. Induction and Aggravation of Pulmonary Heart Disease
Tobacco smoke is a primary causative agent in the development of chronic lung diseases, most notably COPD and emphysema. These conditions lead to chronic hypoxia (low blood oxygen levels), which triggers a cascade of events:
- Pulmonary Hypertension: Chronic hypoxia causes vasoconstriction of the pulmonary arteries, leading to increased resistance in the pulmonary circulation. Over time, structural changes like vascular remodeling and wall thickening further elevate pulmonary arterial pressure, a condition known as pulmonary hypertension (PH).
- Right Ventricular Strain: The right ventricle (RV) is a thin-walled chamber designed to pump blood into the low-pressure pulmonary system. Sustained pulmonary hypertension forces the RV to work against a significantly higher afterload. This leads to right ventricular hypertrophy (thickening of the heart muscle) as an initial adaptive response, followed by right ventricular dilation and eventual right heart failure—the hallmark of pulmonary heart disease.
2. Creating a Substrate for Ventricular Tachycardia
A heart remodelled by PHD provides the perfect arrhythmogenic substrate for ventricular tachycardia. Tobacco smoke accelerates this remodeling process through several mechanisms:
- Myocardial Fibrosis and Remodeling: The chronically strained and hypoxic right ventricle undergoes significant structural changes. Tobacco-derived toxins and systemic inflammation promote the deposition of fibrotic tissue within the ventricular myocardium. This fibrosis disrupts the normal uniform conduction of electrical impulses, creating areas of slow conduction and block. These heterogeneous zones are the foundation for re-entry circuits, the most common mechanism for sustained VT, where an electrical impulse circulates repeatedly around a scarred or fibrotic area.
- Chronic Hypoxia and Acidosis: The systemic hypoxia caused by underlying lung disease affects the entire heart. Hypoxia alters the electrophysiological properties of cardiac cells, affecting ion channel function and reducing the threshold for abnormal automaticity. Furthermore, hypoxia often leads to respiratory acidosis, which can further destabilize cell membranes and promote arrhythmias.
- Autonomic Nervous System Dysregulation: Tobacco smoke contains nicotine, a potent stimulant of the sympathetic nervous system. Chronic sympathetic activation increases heart rate, blood pressure, and myocardial oxygen demand, placing additional stress on the already compromised right ventricle. This constant adrenergic surge also lowers the threshold for ventricular arrhythmias and facilitates triggered activity.
- Oxidative Stress and Direct Cardiotoxicity: Thousands of chemicals in tobacco smoke, including carbon monoxide and reactive aldehydes, generate immense oxidative stress. This oxidative damage directly injures cardiac myocytes, impairs mitochondrial function, and disrupts calcium handling within the cells. Abnormal calcium cycling is a known precursor to delayed afterdepolarizations (DADs), which can initiate triggered VT, especially in a stressed and fibrotic heart.
- Systemic Inflammation: Tobacco use induces a state of chronic systemic inflammation, elevating markers like C-reactive protein (CRP) and various cytokines (e.g., IL-6, TNF-α). Inflammation itself is pro-arrhythmic, contributing to electrical instability and promoting the progression of both pulmonary vascular disease and myocardial fibrosis.
Clinical Evidence and Epidemiological Correlation
Numerous epidemiological studies corroborate the link between tobacco use, PHD, and fatal arrhythmias. Patients with COPD, overwhelmingly caused by smoking, have a significantly higher risk of sudden cardiac death—often due to VT or ventricular fibrillation—compared to the general population. This risk is independent of traditional coronary artery disease risk factors, pointing directly to the pulmonary disease and its cardiac consequences as the primary culprit.
Research has shown that the severity of pulmonary hypertension and the degree of right ventricular dysfunction are strong predictors of arrhythmic events. Ambulatory ECG monitoring in patients with cor pulmonale frequently reveals non-sustained VT, which is a known precursor to sustained, life-threatening episodes. Smoking cessation studies provide the most compelling evidence: patients who quit smoking show a slower progression of lung function decline, improved hemodynamics, a reduction in systemic inflammation, and a consequent decrease in the long-term risk of cardiovascular mortality, including arrhythmic death.
Conclusion and Implications
The connection between tobacco use and an elevated rate of ventricular tachycardia in pulmonary heart disease is unequivocal and mechanistically robust. Tobacco smoke initiates a destructive process that begins in the lungs, culminates in right heart failure, and creates an electrophysiological environment ripe for lethal arrhythmias. It acts through a synergy of hemodynamic stress, structural remodeling, autonomic imbalance, oxidative injury, and pervasive inflammation.
Understanding this intricate relationship underscores the paramount importance of smoking cessation as the most effective intervention to halt disease progression. For clinicians, a high index of suspicion for arrhythmias is essential in managing smokers with underlying lung disease. Beyond quitting, comprehensive management involving supplemental oxygen to correct hypoxia, pharmacological agents to manage pulmonary hypertension, and close cardiac monitoring—including considering implantable cardioverter-defibrillators (ICDs) in high-risk patients—is crucial. Ultimately, combating this cascade requires a relentless focus on primary prevention through global tobacco control initiatives and personalized cessation support, aiming to protect both pulmonary and cardiovascular health from the devastating effects of tobacco.
Tags: #TobaccoAndHeartDisease #PulmonaryHypertension #VentricularTachycardia #CorPulmonale #SmokingCessation #CardiacArrhythmias #COPD #RightHeartFailure #PublicHealth #Cardiology










