Tobacco Smoke: An Aggravating Force in Chronic Sinusitis Headache Intensity
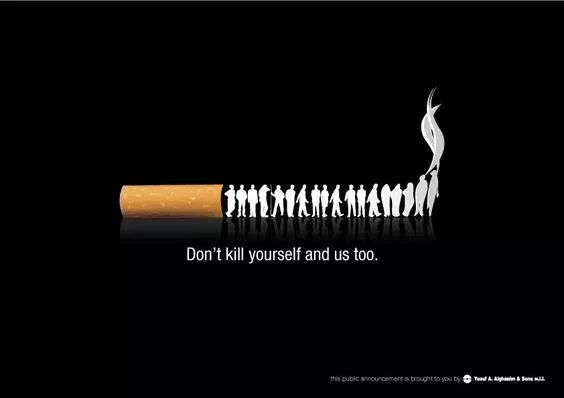
Introduction: The Unseen Aggressor
Chronic sinusitis, a persistent inflammation of the sinuses lasting for more than 12 weeks, is a condition that afflicts millions worldwide. Among its most debilitating symptoms is the relentless, pressure-filled headache that can significantly impair quality of life. While factors like allergies, infections, and anatomical issues are well-known contributors, the role of environmental irritants, particularly tobacco smoke, is often underestimated. This article delves into the compelling evidence and biological mechanisms that establish tobacco smoke as a critical aggravator of chronic sinusitis headache intensity, transforming manageable discomfort into severe, life-disrupting pain.
Understanding Chronic Sinusitis and Its Headaches
To appreciate tobacco's impact, one must first understand the nature of sinusitis headaches. Unlike typical tension or migraine headaches, sinus headaches are caused by the inflammation and blockage of the paranasal sinus cavities. When the sinus linings become inflamed, they swell, preventing normal mucus drainage. This leads to a buildup of pressure that acts directly on the sensitive sinus walls and surrounding nerves, resulting in a deep, throbbing pain typically localized to the forehead, cheeks, and around the eyes. This pressure-sensitive pain is the hallmark of a sinusitis-related headache.
The Chemical Onslaught: How Tobacco Smoke Attacks the Sinuses
Tobacco smoke, whether from active smoking or secondhand exposure, is not a single entity but a complex cocktail of over 7,000 chemicals, including nicotine, tar, formaldehyde, and numerous other potent irritants and carcinogens. This toxic mixture launches a multi-faceted assault on the respiratory system, with the sinuses bearing the initial brunt of the attack.
Firstly, the physical act of inhaling hot, particulate-filled smoke causes direct irritation and drying of the delicate mucous membranes lining the nasal and sinus passages. This disrupts the first line of defense. More critically, these chemicals are potent pro-inflammatory agents. They trigger the release of a cascade of inflammatory cytokines and signaling molecules, which exacerbates the existing inflammation in chronic sinusitis. This leads to further swelling of the sinus tissues, narrowing the ostia (the drainage pathways) even more. The result is a significant escalation in sinus pressure, directly translating to a more intense and severe headache.
Paralyzing the Guardians: Ciliary Dysfunction
One of the most damaging effects of tobacco smoke on sinus health is its impact on the mucociliary clearance system. The sinus linings are equipped with microscopic hair-like structures called cilia, whose constant, wave-like motion is essential for sweeping mucus and trapped pathogens out of the sinuses and toward the back of the throat to be swallowed.
Components of tobacco smoke, notably formaldehyde and hydrogen cyanide, are toxic to these cilia. They paralyze and destroy these vital structures, effectively shutting down the sinuses' self-cleaning mechanism. With the "escalator" broken, mucus stagnates, becomes thicker, and accumulates within the blocked sinus cavities. This stagnation not only increases pressure but also creates an ideal environment for bacterial growth, potentially leading to secondary infections. For the patient, this cilia paralysis means their baseline sinusitis condition worsens, and the accompanying headaches become more frequent, longer-lasting, and far more intense.
Neurological and Vascular Implications
The aggravation of sinus headaches by tobacco is not solely mechanical (pressure-based). Nicotine, the addictive substance in tobacco, is a powerful vasoactive agent. It causes constriction (narrowing) of blood vessels throughout the body. Following this constriction, a rebound dilation (widening) often occurs. In the confined space of the inflamed sinuses, this vascular turbulence can exacerbate swelling and pressure on pain-sensitive structures.
Furthermore, chronic inflammation can sensitize the trigeminal nerve, the primary nerve responsible for sensation in the face and sinuses. This condition, known as peripheral and central sensitization, lowers the pain threshold, meaning normal sensations are perceived as pain (allodynia) and painful stimuli are felt more acutely (hyperalgesia). Tobacco smoke chemicals fuel this neurogenic inflammation, making the nervous system hyper-reactive. Consequently, a patient exposed to tobacco may experience their sinus headache as excruciating due to this amplified neurological response.
Clinical Evidence and Patient Outcomes
The correlation between tobacco smoke and worsened sinusitis symptoms is strongly supported by clinical observation and research. Studies have consistently shown that smokers with chronic sinusitis report more severe symptoms, lower quality of life scores, and a higher frequency of headache complaints compared to non-smokers with the same condition. Imaging studies often reveal more significant mucosal thickening and sinus opacification in smokers.
Perhaps the most telling evidence comes from intervention studies. Patients who successfully quit smoking often report a marked improvement in their sinusitis symptoms, including a notable reduction in the frequency and severity of their headaches. This improvement occurs even without other changes to their treatment regimen, underscoring the direct causative role of tobacco smoke in intensifying their pain.
Conclusion: A Call for Awareness and Action
The link between tobacco smoke and the aggravation of chronic sinusitis headache intensity is clear and mechanistically sound. Tobacco smoke acts as a powerful inflammatory trigger, a paralyzing agent to the sinus' cleansing system, and a disruptor of normal vascular and neurological function. It transforms the challenging reality of chronic sinusitis into a much more painful and debilitating experience.
For healthcare providers, this underscores the critical importance of addressing smoking status with every chronic sinusitis patient. Smoking cessation counseling must be an integral component of treatment plans. For patients, understanding this connection provides a powerful, actionable incentive to quit smoking and avoid secondhand smoke. Eliminating this single aggravating factor can be one of the most effective strategies for reclaiming comfort and reducing the intense pain of chronic sinusitis headaches, paving the way for better overall management of this chronic condition.












