The Lingering Haze: Does Smoking Permanently Alter Taste Perception in Cardiac Patients?
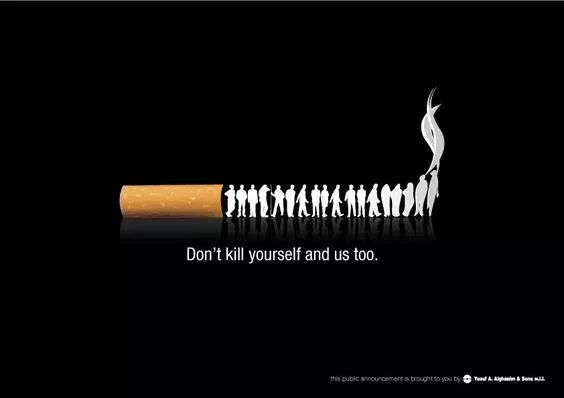
The link between smoking and cardiovascular disease (CVD) is one of the most extensively documented and damning relationships in modern medicine. The detrimental effects of cigarette smoke on the heart, blood vessels, and lungs are well-publicized. However, a more subtle, yet profoundly impactful, consequence often remains in the shadows: the alteration of taste perception. For individuals living with heart disease, who are frequently advised to adopt heart-healthy, low-sodium diets, the ability to taste food accurately becomes not just a matter of pleasure, but a critical component of dietary adherence and overall quality of life. This raises a complex and crucial question: does the damage smoking inflicts on the taste buds of a person with heart disease represent a permanent loss, or is there a path to recovery?
To unravel this, we must first understand the separate and synergistic pathologies that smoking and heart disease impose on the complex sensory system of taste.
The Assault on Taste: A Direct Hit from Smoking
Taste buds, the clusters of sensory cells located primarily on the tongue, are remarkably dynamic structures. They have a short life cycle, regenerating approximately every 10 to 14 days. This inherent regenerative capacity is key to the discussion of permanence. Cigarette smoke is a toxic cocktail of over 7,000 chemicals, including nicotine, tar, hydrogen cyanide, and formaldehyde. This onslaught damages taste buds through several direct mechanisms:
-
Direct Chemical Damage and Keratinization: The hot, toxic chemicals in smoke directly irritate and damage the delicate taste receptor cells. Chronic exposure can lead to a process called keratinization, where the tongue's surface becomes hardened and thickened. This keratin layer acts as a physical barrier, preventing flavor molecules from reaching and stimulating the taste buds effectively. Imagine trying to taste a delicate sauce through a leather glove.
-
Impaired Olfaction (Smell): It is a well-established fact that a significant portion of what we perceive as "taste" is actually derived from our sense of smell. Smoking severely damages the olfactory epithelium in the nasal cavity, dulling the sense of smell. This combined loss of taste (gustation) and smell (olfaction) leads to a profound flattening of the flavor landscape. Foods lose their complexity and become bland.
-
Vascular Constriction: Nicotine is a potent vasoconstrictor, meaning it causes blood vessels to narrow. This reduces blood flow to all tissues, including the tongue. Taste buds, like all living cells, require a rich supply of oxygen and nutrients delivered via the bloodstream to function optimally and regenerate properly. Chronic hypoxia (low oxygen) due to reduced blood flow can stunt the health and renewal of taste cells.
-
Altered Saliva Production and Composition: Smoking can affect both the quantity and quality of saliva. Saliva is essential for dissolving food particles so that taste molecules can be transported to the taste pores. Changes in saliva can further impede this process.
In an otherwise healthy individual, the damage from smoking often manifests as a reduced ability to perceive subtle flavors, a heightened threshold for tasting salt and bitterness, and a general complaint that "food doesn't taste as good as it used to."
The Compounding Factor: Heart Disease and Its Treatments
When heart disease enters the picture, the situation becomes significantly more complex. The damage is no longer just from an external toxin; it is now compounded by the internal pathophysiology of the disease itself and its management.
-
Congestive Heart Failure (CHF) and Edema: In CHF, the heart's pumping efficiency is compromised, leading to fluid buildup in tissues, a condition known as edema. This edema can occur systemically, including in the tongue. Swelling of the tongue can physically distort taste buds and affect the taste pores, further impairing function.
-
Medication Side Effects: The pharmacological arsenal against heart disease is extensive, and many common medications are notorious for causing taste disturbances, a condition known as dysgeusia. Drugs such as certain angiotensin-converting enzyme (ACE) inhibitors, statins, and diuretics can cause a metallic, bitter, or simply bland taste in the mouth. For a smoker with heart disease, this iatrogenic effect layers on top of the smoke-induced damage.
-
Chronic Systemic Inflammation and Oxidative Stress: Both smoking and heart disease are pro-inflammatory states characterized by high levels of oxidative stress. This systemic inflammation can negatively affect nerve function and cellular health throughout the body, including the nerves that carry taste signals to the brain.
Permanence versus Plasticity: The Critical Question
So, is the damage permanent? The answer is nuanced and hinges on one primary factor: smoking cessation.
The human body possesses a remarkable capacity for healing, and the taste system is no exception. Because taste buds are in a constant state of renewal, removing the source of the damage—cigarette smoke—allows for a significant degree of recovery. Studies on smokers who quit consistently show an improvement in taste sensitivity over time. The keratinized layer on the tongue can slough off, allowing new, healthy taste buds to emerge. Olfactory function can also improve as the inflammation in the nasal passages subsides.
However, the term "permanent" must be considered in the context of cumulative and long-term damage. An individual who has smoked heavily for several decades, particularly one with advanced heart disease, may not experience a complete return to a pre-smoking level of taste acuity. The cumulative insult may have caused some degree of irreversible damage to the olfactory nerves or the taste bud stem cell population. Furthermore, if heart disease has led to chronic conditions like persistent tongue edema or if the patient must remain on medications that alter taste, a full recovery may be hindered.
Therefore, while the damage is often not absolutely permanent in the sense that there is zero recovery, it can be functionally permanent if smoking continues. For the patient with heart disease, continued smoking ensures a continuous cycle of damage that overwhelms the body's regenerative capabilities. The combination of smoke, disease, and medication can create a lasting deficit.
Implications for Cardiac Rehabilitation and Quality of Life
This has profound implications. A heart-healthy diet is central to managing CVD. It is typically low in sodium, saturated fats, and processed sugars. If food tastes bland and unappealing due to impaired taste, patient adherence to these dietary guidelines plummets. The temptation to over-salt food or revert to unhealthy, highly processed options that are engineered to be palatable despite taste deficits becomes strong. This can directly undermine medical treatment, leading to worse health outcomes and a reduced quality of life.
Conclusion: A Call for Integrated Care
In conclusion, smoking does not necessarily cause absolute permanent damage to the taste buds in people with heart disease, but it creates a high risk for functional permanence, especially if the habit persists. The regenerative power of the taste system offers a beacon of hope, but this hope is entirely contingent upon smoking cessation.
This underscores the critical need for smoking cessation programs to be an integral, non-negotiable component of cardiac rehabilitation. Healthcare providers must not only advise patients to quit but also educate them about the sensory benefits of doing so. Framing smoking cessation as a way to "reclaim the joy of eating" and making dietary adherence easier can be a powerful motivator alongside the more prominent messages about heart attacks and cancer. For the cardiac patient, restoring taste is not a trivial matter of gastronomic pleasure; it is a vital step towards reclaiming health and vitality, one flavorful, heart-healthy meal at a time. The path to recovery is challenging, but the first and most crucial step is to clear the haze, allowing the senses, and the body, to heal.










