Title: The Impact of Smoking on Ventilatory Function: How Tobacco Lowers Maximum Ventilation Volume to Predicted Ratio
Introduction
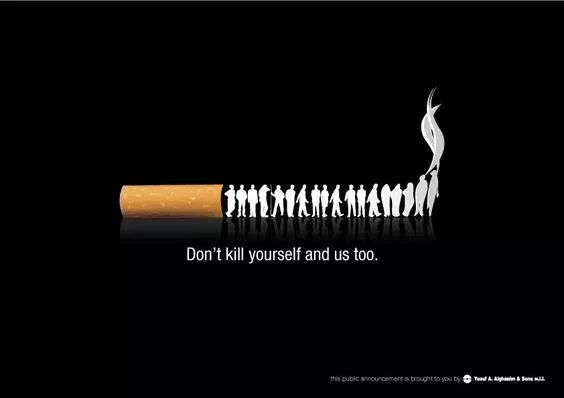
Smoking remains one of the most significant public health challenges worldwide, contributing to a range of respiratory, cardiovascular, and oncological diseases. Among its many detrimental effects, smoking profoundly impairs lung function, particularly by reducing the Maximum Ventilation Volume (MVV) to Predicted Ratio. This ratio, often expressed as a percentage, compares an individual’s actual MVV—the maximum amount of air a person can inhale and exhale per minute during forced breathing—to the predicted value based on age, sex, height, and ethnicity. A lower MVV-to-predicted ratio indicates compromised ventilatory capacity, which is closely linked to respiratory diseases such as chronic obstructive pulmonary disease (COPD), asthma, and emphysema. This article explores the mechanisms through which smoking lowers this critical ratio, its clinical implications, and the broader context of tobacco-induced lung damage.
Understanding Maximum Ventilation Volume and Its Predictive Value
The Maximum Ventilation Volume (MVV) test is a key component of pulmonary function testing (PFT). It measures the maximum voluntary ventilation achieved over a short period, typically 12–15 seconds, and extrapolates it to one minute. The predicted MVV is derived from standardized equations that account for demographic and physiological factors. A normal MVV-to-predicted ratio ranges from 80% to 120%, with values below 80% suggesting ventilatory impairment. This ratio is crucial for diagnosing obstructive and restrictive lung diseases, assessing preoperative risk, and evaluating overall respiratory health.
How Smoking Affects Lung Function
Cigarette smoke contains over 7,000 chemicals, including nicotine, tar, carbon monoxide, and numerous carcinogens. These substances inflict damage through multiple pathways:
- Airway Inflammation and Irritation: Smoke particles trigger chronic inflammation in the airways, leading to swelling, mucus hypersecretion, and bronchoconstriction. This narrows the air passages, increasing resistance to airflow and reducing MVV.
- Ciliary Dysfunction: The cilia lining the respiratory tract are paralyzed and destroyed by tobacco smoke, impairing mucus clearance. This results in chronic bronchitis, a condition characterized by coughing and sputum production, which further obstructs ventilation.
- Parenchymal Damage: Smoke induces oxidative stress and protease-antiprotease imbalances, causing alveolar destruction and emphysema. This reduces lung elasticity and gas exchange surface area, diminishing the force and efficiency of ventilation.
- Muscular Fatigue: Smoking contributes to respiratory muscle weakness by reducing oxygen delivery and promoting systemic inflammation, limiting the ability to sustain high ventilation rates.
Evidence of Reduced MVV-to-Predicted Ratio in Smokers
Numerous studies have demonstrated that smokers exhibit significantly lower MVV-to-predicted ratios compared to non-smokers. For instance, a longitudinal study published in the American Journal of Respiratory and Critical Care Medicine found that current smokers had an average MVV ratio of 65–75%, compared to 85–95% in never-smokers. The decline is dose-dependent, correlating with pack-years (number of packs smoked per day multiplied by years of smoking). Even light smokers show early signs of reduction, highlighting the sensitivity of MVV to tobacco exposure.
Clinical Implications and Disease Progression
A lowered MVV-to-predicted ratio is often an early marker of smoking-related lung disease. It precedes more severe conditions like COPD, where the ratio can drop below 50%. This reduction compromises exercise tolerance, leading to dyspnea (shortness of breath) and reduced quality of life. Additionally, a low MVV ratio is associated with increased perioperative complications, as it reflects diminished respiratory reserve. In advanced stages, it correlates with higher mortality rates from respiratory failure.
Reversibility and Prevention
Quitting smoking can partially reverse ventilatory impairment. Studies indicate that within one year of cessation, MVV values may improve by 5–10%, though recovery is often incomplete due to irreversible structural damage. Preventive measures, including public health interventions like smoking bans, education campaigns, and nicotine replacement therapies, are essential to curb the decline in lung function.
Conclusion
Smoking systematically lowers the Maximum Ventilation Volume to Predicted Ratio through inflammatory, obstructive, and destructive mechanisms. This reduction serves as a critical indicator of ventilatory decline and heightened disease risk. Addressing tobacco use remains paramount to preserving lung health and mitigating the global burden of respiratory diseases.
Tags: #Smoking #LungFunction #MVV #RespiratoryHealth #COPD #PulmonaryMedicine #TobaccoEffects #VentilationRatio #HealthScience #PreventiveCare










